Case Competition 2024 – All submitted cases Case 9 Unconventional Reconstruction of a Complex Genital Defect
Keywords: Genital reconstruction, DIEP flap, Rotation flap
Authors: Iman Ghanad (MD) and Amir K. Bigdeli (MD). BG Ludwigshafen, Germany
A 56-year-old male patient presented to the urological emergency department with progressively increasing swelling and redness in the genital area. Following the diagnosis of Fournier gangrene, the patient underwent multiple radical necrosectomies, bilateral hemiscrotectomies, and surgical displacement of the testicles into femoral scrotal compartments. Septic symptoms and acute kidney failure necessitated intensive care monitoring for the first sixteen days postoperatively. Subsequently, a significant soft tissue defect (17 x 24 cm) in the inguinal and genital region emerged, prompting referral to our hospital for specialized defect reconstruction. The patient’s medical history revealed several underlying conditions including coronary artery disease, arterial hypertension, and type II diabetes mellitus with polyneuropathy. Initially, wound bed preparation was performed in our clinic for further reconstructive planning. It was noticed that the wound was suitable for split-thickness skin grafting. However, due to the patient’s non-compliance and the necessity for postoperative bed rest, which the patient did not adhere to, the attempts at split-thickness skin grafting were futile on two occasions. Consequently, the patient decided to discharge himself voluntarily against explicit medical advice. Due to postoperative bleeding and persistent wound healing issues, the patient returned to our clinic for further surgical treatment.


Before and after
Patient examination
Upon admission to our hospital, the 56-year-old male exhibited obesity. A 17 x 24 cm soft tissue defect could be identified in the inguinal and genital area with bilateral exposed testicles. The testicles were previously relocated into subcutaneous pouches in the thighs. No signs of infection could be detected.
Pre-Operative Considerations
Reconstructive surgery encounters a significant challenge when addressing complex soft tissue loss in the genital and inguinal regions. The inguinal area represents a crucial convergence point of essential anatomical structures. Several individual factors need consideration in developing the treatment plan, including the extent of the defect, potential exposure of anatomical structures, functional requirements, and the patient’s medical history. Given the patient’s prior non-compliance with strict bed rest, opting for free flap surgery carries a heightened risk of failure. Furthermore, previous attempts at split-thickness skin grafting were unsuccessful. Considering the size and position of the soft tissue defect, along with the patient’s specific circumstances of prior unsuccessful coverage attempts, we chose to perform defect reconstruction using a sliding triangular-shaped Deep inferior epigastric perforator (DIEP) flap. Alternatively, there was the option of reconstruction using bilateral Anterolateral thigh (ALT) flaps. Preoperative CT angiography and color-coded duplex sonography demonstrated robust medial abdominal perforators. Following preoperative surgical treatment plan was worked out for a one stage surgical attempt:
- 1. Extensive debridement of the wound bed to remove previously epithelialized skin areas due to the conducted split-thickness skin grafting.
- 2. Reconstruction of the soft tissue defect with a triangular-shaped DIEP flap.
- 3. Alternative: Reconstruction of the soft tissue defect using bilateral unipedicled ALT flaps.

Step 1: Previous multiple wound bed preparation and skin Grafting attempts

Step 2: Intra-operative Planning
The initial intraoperative plan was to raise a triangular-shaped bipedicled DIEP flap, intending to rotate it 90° clockwise to reconstruct the entire defect, encompassing both the testicles and scrotum

Step 3: Extensive Debridement

Step 4: Flap dissection:
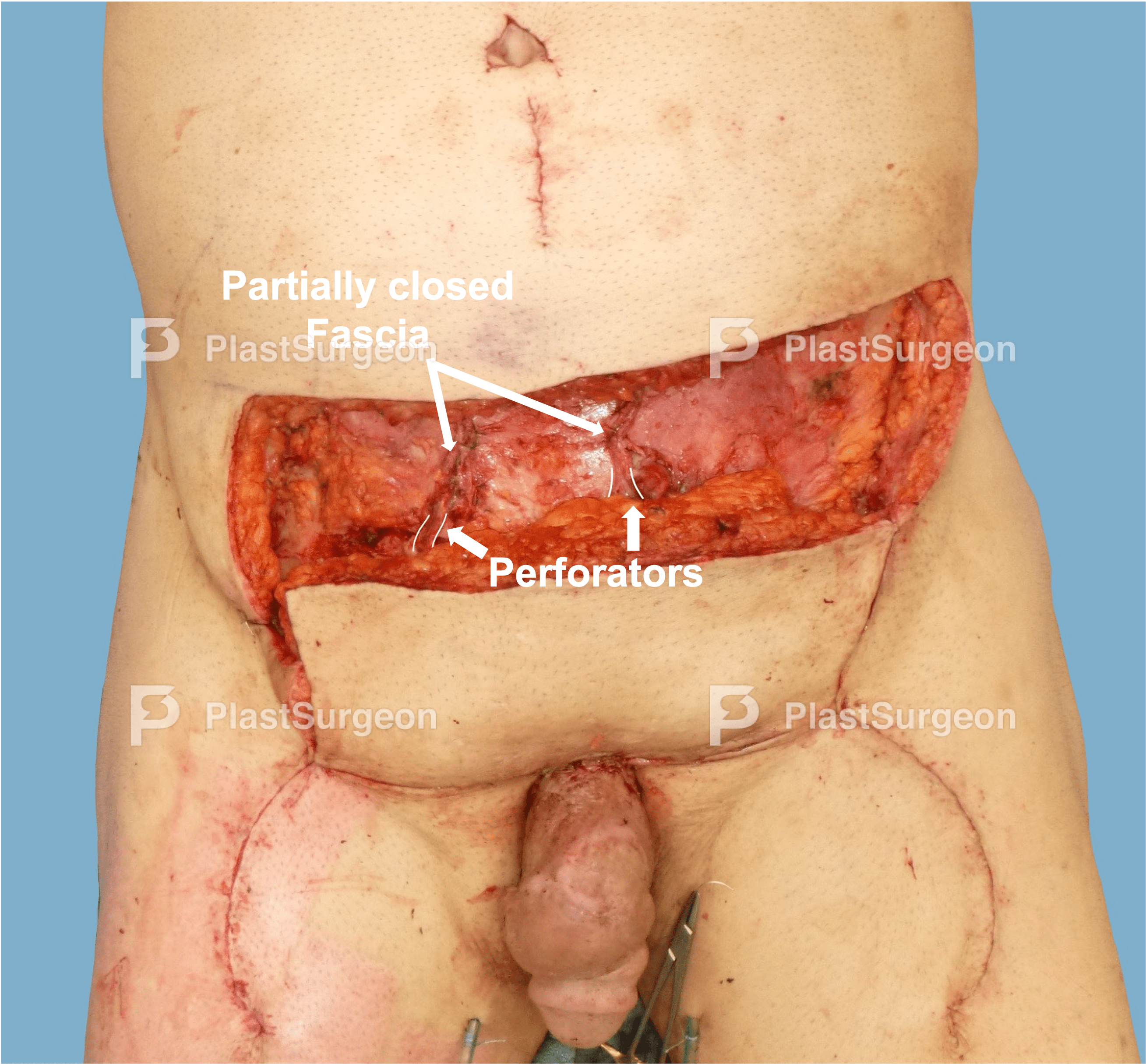
Following a meticulous analysis of the flap dimensions and the extent of the defect, we revised our initial reconstruction plan. Considering the dimensions of the defect, we chose to perform proximal defect reconstruction using a sliding bipedicled DIEP (Deep Inferior Epigastric Perforator) flap for the proximal portion of the defect. Additionally, we decided to reconstruct the distal portions of the defect using rotational flap surgery from the inner thighs.

Step 5: Dissection of the rotational flaps for reconstruction of the distal defect:
At the beginning, the borders of the rotational flap were delineated and marked on both sides of the thigh using a sterile marker. Following the preparation and elevation of the rotational flap, rotation was executed along with additional release in the form of bilateral Burow’s triangles. Through this method, the rotational flap successfully achieved tension-free coverage of the distal skin and soft tissue defect up to the base of the penis. The flaps were attached to the remaining scrotum with 3-0 absorbable sutures.

Step 6: Dissection of the DIEP flap for reconstruction of the proximal defect:
The borders of the DIEP flap were delineated and demarcated according to the needed size, using a sterile marker. For the reconstruction of the remaining defect, a DIEP flap reconstruction was performed, incorporating the robust medial perforators previously identified in the CT-Angiography. Initially, the right-sided DIEP flap was elevated from lateral to medial in an epifascial manner. Subsequently, the left-sided flap was then elevated

Step 7: Perforator identification and dissection:
The procedure involved precise dissection of the large-caliber epigastric perforators of the medial row and tracking them through the muscle. The perforators were dissected until tensionless sliding of the flap was possible. In this process, the muscle remained almost entirely intact. Subsequently, the flap was perfused adequately only through the perforators after sufficient dissection.

Step 8: Distal transposition of the flap
Following the adequate preparation of the perforators, the flap was shifted distally.
Step 9: Modelling:
Now, the tension-free caudal shift of the flap was performed. Furthermore, the umbilicus was repositioned more caudally. Limited mobilization of the abdominal wall was conducted to ensure a tension-free closure.

Step 10: Securing of flap
Securing the DIEP flap and donor-site closure:Donor-site closure was achieved through a modified abdominoplasty. Securing of the flap was performed with self-resorbing subcutaneous and intracutaneous sutures. The abdominal fascia was closed with non-resorbale Prolene 2-0 sutures without constriction of the perforators on both sides.
Post-Operative Plan
The patient should remain sedentary in bed for five days with hourly monitoring of the perfusion of the flaps by the surgeon for 48 hours. The patient will require outpatient monitoring and follow-up appointments scheduled at two weeks, six weeks, three months, and 12 months post-surgery.
- The unconventional use of bipedicular sliding DIEP flap may achieve outstanding results in covering complex genital defects.
- Extensive preoperative planning can streamline the surgical procedure and decrease the duration of the operation.
- Non-Compliance can severely limit the options for defect reconstruction.
- Tension-free flap surgeries are crucial for successful healing




































